The health authorities created a five-kilometer surveillance zone surrounding the afflicted area by the Zika virus.
Table of Contents

Breaking News of Zika threat:
Health officials quickly launched a number of actions to address and contain the situation after confirming a positive Zika virus case in the Sidlaghatta area, which is situated within the Talakayala Betta region of Dibburahalli in the Chikkaballapur district of Karnataka. Recognising the virus’s presence in the area, the District Health Officer (DHO) issued an alert, prompting an instant reaction from the health department in D1.
Proactively attempting to stop the virus from spreading, the health authorities created a five-kilometre surveillance zone surrounding the afflicted area. The purpose of this perimeter was to keep a close eye on any possible spread of the virus from its original site.
Officials in the department were quickly called to an urgent meeting after realising how urgent the situation was. After the worrying news of the confirmed Zika case, this meeting provided a forum for planning and implementing a successful response strategy. The plan’s objectives were to stop the disease from spreading, offer the required medical care, and guarantee the community’s safety.
Following an analysis of mosquitos in Chikkaballapur, Karnataka, media sources suggest the existence of the Zika virus. Health officials identify a single Zika incidence in the district, indicating extra vigilance. The Chikkaballapur tragedy emphasises the significance of taking preemptive measures to prevent the virus from spreading. To prevent additional transmission, authorities are expected to step up mosquito control measures and public awareness programs.
It is critical to respond quickly and effectively to Zika epidemics in order to safeguard both afflicted people and the larger society. To reduce the effect of the Zika virus in the region, healthcare experts, government entities, and the general public must work together. Chikkaballapur District Health Officer (DHO), SS Mahesh stated to the media, that “Out of a total of 100 samples collected across the state, six were from Chikkaballapur. While five of them tested negative, one person has been confirmed positive for the virus”.
The results of the test of virus:
The District Health Officer (DHO) reports that blood samples from 30 pregnant women and seven individuals with fever symptoms have been sent for testing, with final results awaited. The DHO highlights the need for proactive health monitoring, advising people who have had high temperatures for three days in a row to produce blood tests. This effort attempts to identify and manage any health risks as soon as possible, particularly among pregnant women.
The results of the forthcoming tests will be critical in identifying and managing the community’s health challenges, emphasising the importance of prompt and collaborative public health measures.
Origin of the virus and its symptoms:
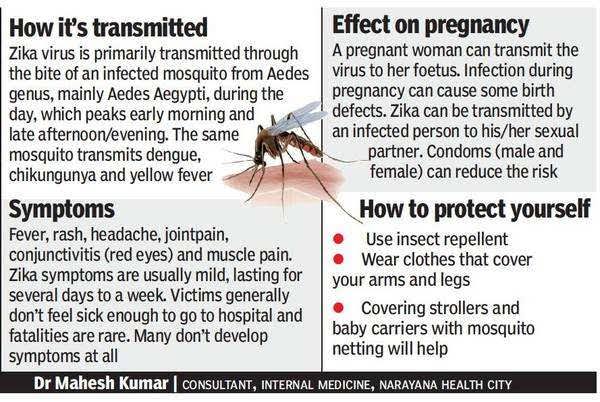
Zika virus, originating in Uganda in 1947, transitioned from sporadic cases to global outbreaks in 2007, spanning Africa, the Americas, Asia, and the Pacific. Linked to Guillain-Barré syndrome and microcephaly, the virus prompted a WHO Public Health Emergency in 2016. Zika’s decline globally after 2017 hasn’t eradicated it; low-level transmission persists in the Americas and other regions. Notably, Europe reported local cases in 2019, and an outbreak occurred in India in 2021. With 89 countries affected, surveillance challenges persist despite the diminished prevalence, according to WHO.
Many people infected with Zika suffer no symptoms, while others get moderate symptoms such as rash, fever, and joint discomfort. These symptoms, which typically present 3-14 days after infection and persist for 2-7 days, overlap with a variety of disorders. Due to similarities with other arboviral and non-arboviral diseases, precise diagnosis needs laboratory confirmation. Vigilance is advised in the face of an unseen threat.
How fatal is the Zika virus?
Zika virus poses severe risks during pregnancy, leading to microcephaly and congenital malformations like limb contractures and hearing loss, collectively termed congenital Zika syndrome. The extent of risk for malformations remains uncertain, with 5-15% of infants from infected pregnancies displaying complications. Both symptomatic and asymptomatic infections contribute to congenital malformations, alongside potential complications like fetal loss and preterm birth.
What should we do:
What makes the Zika virus fatal is, that there is neither any treatment nor any vaccine to control this virus. However, if diagnosed early, the symptoms can be less fatal. However, diagnosis of Zika virus infection requires laboratory testing on blood or other bodily fluids. Distinguishing it from closely similar flaviviruses such as dengue, against which the patient may have been exposed or immunized, is critical to the approach. Precision in distinction guarantees correct identification.



